A particularly vexing complication of cataract surgery is thermal damage to the corneal incision. Causes include occlusion of the phaco needle, handpiece, or aspiration tubing by hard nuclear material and low fluid flow because of a tight wound or OVD blockage of the phaco needle.
A thermal burn produces corneal changes ranging in severity from mild opacification of the corneal tunnel to several millimeters of wound gape, which can result in leakage and anterior chamber collapse.1 Thankfully, the development and adoption of advanced phaco power modulation programs and femtosecond laser technology to presoften and divide a cataract have made this complication rare. Its infrequency, however, means that many surgeons have little experience with closure techniques.
As noted by Robert J. Weinstock, MD, if plumes of white smoke appear in the anterior chamber during the application of phaco power and the nucleus is not dissolving, occlusion has likely occurred. In this event, phacoemulsification should be halted and the handpiece flushed.2 Unfortunately, collagen contraction has probably already occurred.
Even a small wound gape is hard to seal with traditional hydration techniques, and one or more interrupted 10-0 sutures may be required to close the incision. Robert H. Osher, MD, has described two closure techniques.3,4 One is a radial suture between the anterior and posterior portions of the incision. The other is a horizontal gape suture, which is a trapezoidal mattress suture approximating the anterior floor to the posterior roof. Both strategies are effective for small gapes, but they can induce astigmatism. For large gapes and persistent Seidel-positive leakage, many surgeons apply a tissue adhesive and ask patients to tolerate 3.00 to 5.00 D of astigmatism.
I propose an alternative. For gaping that is severe enough to require suture compression, which would cause corneal striae and with-the-rule astigmatism, I have developed a wound gape transposition technique that produces a watertight closure with little or no induced astigmatism and no need for a tissue adhesive.
SURGICAL TECHNIQUE
This suturing strategy transfers the gape from the cornea to nearby sclera. Even with a large gape, cataract removal can be completed and the IOL implanted under an OVD.
Before removing the OVD—a step that will collapse the anterior chamber—I instill acetylcholine in the anterior chamber to constrict the pupil and prevent IOL-cornea touch. While waiting for the pupil to constrict, I make a conjunctival peritomy to expose sclera posterior to the wound gape and perform wet field cautery to gently blanch potential bleeders.
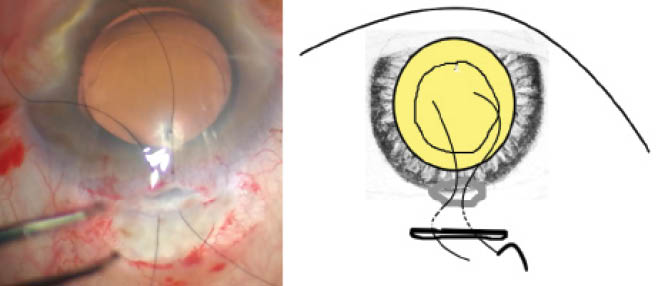
Figure 1 | Before removing the OVD, the surgeon injects carbachol intraocular solution (Miostat, Alcon) into the anterior chamber. Several interrupted sutures are passed through the anterior edge of the corneal incision and through the posterior edge of the corneal incision, after which they are tunneled through the sclera and exit through the scleral incision, which is approximately 50% longer than the corneal incision.
Next, I make a scleral incision that is approximately 50% longer than the corneal incision (eg, 4 mm for a 2.6-mm corneal incision, Figure 1). The scleral incision is located 2 mm posterior to the corneal incision, and its depth is at least half the scleral thickness. A 10-0 nylon suture (or a 9-0 nylon suture for large gapes) is passed through the anterior edge of the corneal incision and through the posterior edge of the corneal incision, after which it is tunneled through the sclera and exits through the scleral incision. A healthy length of suture may be left in place, and a second or even a third pass with the remaining suture material may be made and left in place. (Preplacing sutures makes it easier to close the incision if the iris prolapses after the OVD is removed.)
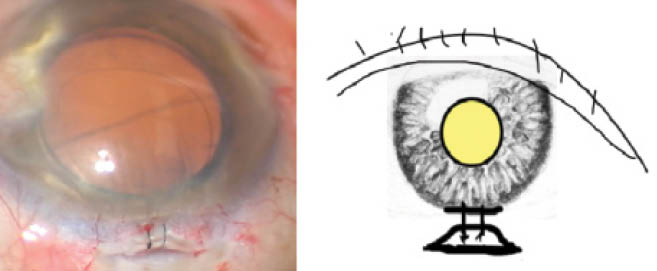
Figure 2 | Immediately after removing the OVD, the surgeon ties the interrupted sutures tightly. The wound gape should be totally transferred from the cornea to the sclera with little or no astigmatic effect.
I remove the OVD from behind and in front of the IOL. Immediately after the irrigation tip has been removed and the anterior chamber collapses, I tie the interrupted sutures as tightly as necessary to close the corneal gape and then refill the anterior chamber with balanced salt solution (Figure 2). The knots are buried, and the conjunctiva is closed with wet-field cautery.
This process should totally transfer the gape from the cornea to the sclera with little or no astigmatic effect. The partial-thickness scleral defect should granulate in during healing.
Phaco burns seldom occur, but over the years this technique has served me well when one has.
1. Sugar A, Schertzer RM. Clinical course of phacoemulsification wound burns. J Cataract Refract Surg. 1999;25(5):688-692.
2. Kent C. Managing surgical complications. Review of Ophthalmology. March 5, 2014. www.reviewofophthalmology.com/article/managing-surgical-complications. Accessed June 1, 2020.
3. Osher RH. Gape closure. Video Journal of Cataract and Refractive Surgery. 1990;6(3). https://eyetube.net/series/video-journal-of-cataract-and-refractive-surgery/video.asp?vol=06&iss=3&f=gape-closure. Accessed June 1, 2020.
4. Osher RH, Osher JM. Wound gape: two closure techniques. Cataract & Refractive Surgery Today. June 2011. https://crstoday.com/articles/2011-jun/wound-gape-two-closure-techniques. Accessed June 1, 2020.



