With most international travel cancelled this year due to COVID-19, many medical missions have been unable to proceed as planned. Some organizations, however, are now taking the opportunity to evaluate and evolve their practices in order to better provide global ophthalmic care in this new reality. This article is part one of a series exploring the different ways that global ophthalmology has been affected by the COVID-19 pandemic and how those involved with international medical missions are adapting their efforts during this unprecedented time.
Orbis International’s Flying Eye Hospital
Goes Virtual
At the onset of the COVID-19 pandemic, Orbis International made the difficult decision to postpone its Flying Eye Hospital programs through the end of this year, including planned trips to Zambia, Cameroon, Mongolia, and India.
Orbis has more than 400 volunteer faculty members from over 30 countries who work to achieve the organization’s mission to help local eye care teams improve the level of care they can provide for future generations. These volunteers, which include ophthalmologists, nurses, anesthesiologists, and biomedical engineers, share their skills with local eye care teams around the world. This is primarily done by providing training to partner hospitals through Orbis’ telemedicine platform Cybersight, on site at the partner hospitals, and on the Flying Eye Hospital—the world’s only fully accredited ophthalmic teaching hospital on board an MD-10 aircraft (Figure 1).
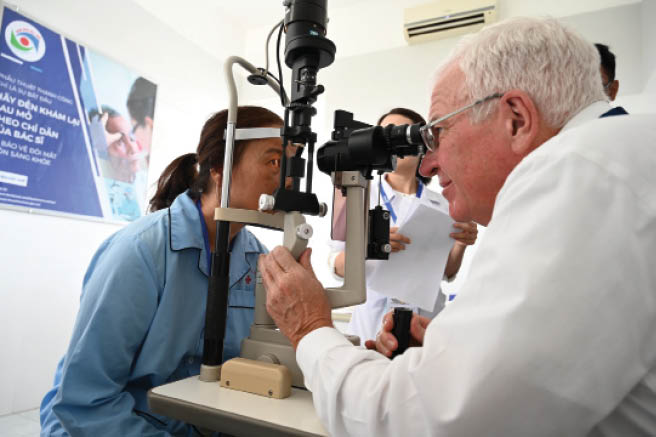
Figure 1 | Dr. Alward during his sixth Flying Eye Hospital program in Hue, Vietnam, in 2019.
Although the Flying Eye Hospital is temporarily grounded, Orbis’ mission is not. In May, Orbis launched its virtual Flying Eye Hospital training program for eye care professionals in Zambia who were due to receive in-person training (Figure 2). A remote curriculum tailored to the training needs of more than 100 Zambian providers, including doctors, nurses, biomedical engineers, and technicians, was created and delivered through Cybersight. Orbis also launched an additional virtual Flying Eye Hospital program for more than 90 eye care professionals in Cameroon. We also look forward to offering these programs for eye care professionals in Mongolia and India this year and hopefully for other locations in the future as well.
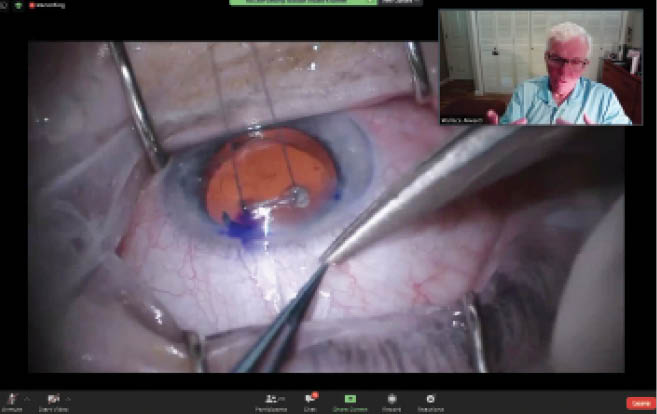
Figure 2 | Dr. Alward during Orbis International’s inaugural virtual Flying Eye Hospital training program for eye care professionals in Zambia.
The curriculum of every Orbis training program is tailored to meet the needs of the participating local eye care professionals. Planning for a Flying Eye Hospital program is a process that starts more than a year in advance, in coordination with partner hospitals with which Orbis has long-standing relationships. Because the virtual Flying Eye Hospital programs launched this year have served eye care professionals who were originally going to train in person, the education they have been offered online has been informed by that meticulous preparation. In Zambia, for example, Orbis has been working with partner institutions in the country for years and has a country office and permanent staff on the ground; therefore, the Flying Eye Hospital program—whether in person (Figure 3) or virtual—offers an opportunity to build on prior training sessions.

Figure 3 | Dr. Alward with eye care trainees on the Flying Eye Hospital in Hue, Vietnam, in 2019.
COVID-19’S EFFECT ON GLOBAL OPHTHALMIC CARE
Amid the lockdowns in the early stages of the pandemic, most ophthalmologists around the world were seeing only emergency cases, such as patients with suspected cancer or traumatic eye injury. As a result, many patients missed their routine check-ups. Because glaucoma is a chronic disease, there is a danger that high IOP went undetected or uncontrolled during the lockdown and caused irreversible damage. It is possible that we still have not seen the full extent of those effects.
Going forward, we do not want patients to forgo visits to their eye care clinics or refrain from picking up their IOP-lowering medications from the pharmacy because they are concerned about COVID-19. We should all take the necessary precautions and prioritize safety, and we emphasize this often to our partner hospitals. However, a chronic disease such as glaucoma does not stop progressing because there is a pandemic.
Fortunately, patients are slowly returning for in-person care, and many of our partner hospitals around the world are looking to Orbis for guidance on safety protocols as they reopen. In response, Orbis has launched a library of resources on Cybersight that cover the topic of reopening—one more way in which the organization is virtually meeting the challenges presented by COVID-19.
AI Tools on Cybersight
Orbis International has an open-access AI tool on Cybersight (www.cybersight.org) that can detect and visualize glaucoma from fundus photographs in just a few seconds. Because glaucoma can be difficult to diagnose, Cybersight users can choose to have a mentor doctor talk them through the machine’s findings and help them establish a diagnosis. In this way, Orbis is teaching eye care professionals how to better identify signs of glaucoma in their patients. Orbis also offers similar AI tools for the detection of macular disease and diabetic retinopathy.
The price point of cutting-edge technologies such as AI have too often kept them out of reach for the eye care professionals who need them most. For that reason, Orbis is working to democratize AI and ensure that eye care professionals in low- and middle-income countries can access these tools for free through Cybersight.
A VITAL RESOURCE
Since the pandemic started, Cybersight’s number of registered eye care professionals has grown by more than 200%. Ophthalmology residents who have been unable to return to their institutions for traditional in-person training have said that Cybersight has been a fantastic training resource during this time. Users have appreciated the ability to tailor their learning by combining our synchronous and asynchronous offerings.
Additionally, eye care professionals from Zambia who completed the virtual Flying Eye Hospital program said that the courses improved their knowledge and that they would recommend the courses to their colleagues. They all showed interest in participating in additional online courses and requested more live educational sessions.
Of course, virtual training is not without its challenges. One of the biggest barriers to virtual training relates to the lack of human interaction, which affects both relationships and learning—for example, by eliminating the ability to shake someone’s hand or provide hands-on support to demonstrate a technique. In addition, we miss out on working alongside other volunteer faculty and Orbis staff members as well as the local nurses, technicians, anesthesiologists, and bioengineers.
With virtual learning, we do not have the opportunity to get to know the people we are teaching in the same way we would in person. Many cultures are more formal than ours, and training participants can be reluctant to ask questions of their teachers. On site, we can more easily befriend the participants and help them to grow comfortable engaging in dialogue, perhaps over lunch in the cargo hold of the Flying Eye Hospital. By working alongside our participants, Orbis volunteer faculty members also have the chance to gauge the gaps in knowledge that need to be addressed.
In the case of the virtual Flying Eye Hospital programs, Orbis has been able to mitigate some of these challenges due to our existing relationships with local eye care professionals and/or partner hospitals. We are aware of their educational needs and know what equipment they can access in their local facilities. Additionally, these programs fit in seamlessly with existing blended learning models we have been running with partners around the world since long before the pandemic started.
VIRTUAL TRAINING NOW AND IN THE FUTURE
Orbis has a long history of using virtual solutions to ensure that eye care professionals in low- and middle-income countries can access quality training. This enabled us to pivot our approach quickly and seamlessly at the start of the pandemic. The virtual Flying Eye Hospital programs leverage the virtual training that Orbis has been leading through Cybersight.
Cybersight was launched in the early days of the internet, and it has become a 24/7 virtual training hub where eye care professionals can access courses, books, and live lectures. Although the platform was designed to bring free training and mentoring to eye care professionals in low- and middle-income countries, we have been pleasantly surprised to see the uptake of our course offerings by doctors in high-income countries such as the United States, Canada, and the United Kingdom.
When in-person visits are once again feasible, we look forward to making virtual training a long-term component of our Flying Eye Hospital programs through blended learning. For example, we may use virtual education to provide pre-learning before the plane arrives or to build on in-person training after the plane departs. We believe this will permit a more in-depth educational experience.
CONCLUSION
For a long time, Orbis has run its programs with the understanding that telemedicine and remote learning are the tools of the future. COVID-19 has accelerated their mainstream acceptance and uptake, and they are here to stay. In the current age of social distancing, telemedicine and remote learning have taken the place of Orbis’ in-person trainings, but they are not simply a stopgap measure to get us through the pandemic. The ways in which we are adapting and learning today build on our long history of innovation and will enhance how we run both our virtual and in-person programs in the future.




