Placement of a secondary IOL is one of the most gratifying procedures for both the ophthalmic surgeon and the patient. A sutured approach to scleral fixation using polypropylene or Gore-Tex and sclerotomies or Hoffman pockets is an elegant, simple procedure. However, the large incision size required for some lenses, such as my preferred CZ70BD IOL (Alcon), and the long-term risk of suture erosion through the sclera or conjunctiva make these techniques undesirable in many cases.
THE YAMANE TECHNIQUE
The introduction of the Yamane technique for intrascleral haptic fixation, developed by Shin Yamane, MD, has simplified scleral fixation and decreased visual recovery time due to smaller incision size and sclerotomies. By avoiding a large scleral tunnel, the risk of postoperative hypotony is negligible. Also, because a conjunctival peritomy is not required in most cases, conjunctival manipulation is minimized in patients who often have limited healthy tissue. For me, transitioning to the Yamane technique for intrascleral haptic fixation was game-changing.
In perfect cases, the procedure is graceful and smooth—a result that is easily achievable after an initial learning curve to identify the ideal incision placement and instrumentation. On the contrary, cases of fully vitrectomized eyes, in which iris support for the IOL during the beginning steps of the procedure is limited, can quickly become exceptionally challenging.
One of the most anxiety-inducing moments during these cases is after injection of a three-piece IOL into the anterior chamber, as there is limited barrier keeping the lens from falling into the depths of the vitreous cavity. After a few close calls in which the IOL was a little too close to falling from the anterior chamber, I eventually had the misfortune of watching a lens drop like a rock to the vitreous cavity, far out of my reach.
Luckily, I operate in a facility where there is almost always a skilled retina surgeon nearby, available and willing to assist when needed. With the help of my colleague, the lens was retrieved (Figure 1) so that I could have a second try at fixation. Ultimately, the patient did very well, but only after more surgical manipulation and angst than preferred.
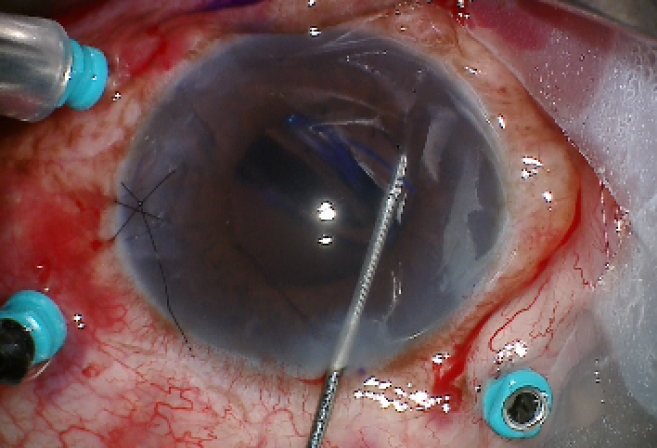
Figure 1 | IOL after retrieval from the vitreous cavity.
LESSONS LEARNED
During my next case, due to my previous misfortune and an almost-entirely absent iris, I decided to use an IOL glide to support the lens after its insertion into the anterior chamber. This helped stabilize the IOL during sclerotomy creation and docking of the leading haptic (Figure 2). The procedure went well, despite the lack of anterior chamber support.
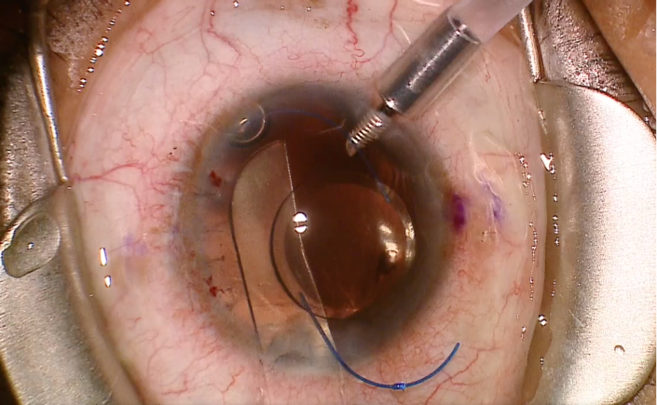
Figure 2 | IOL supported by a glide prior to scleral fixation in an eye with traumatic aniridia.
The IOL glide serves as a platform to support the lens during the initial and critical steps, and it eliminates the need for a skilled third hand, which is almost always desired but often unavailable. This is a modification that I employ in all cases of significant traumatic mydriasis or iris loss, and it has greatly reduced my stress and concern regarding dropped IOLs.



